RCT Comparing LVA vs. CDT: A 6 month interim analysis
- Dec 1, 2025
- 3 min read
Authors: Jonis YMJ, Wolfs JAGN, Hummelink S, Tielemans HJP, Keuter XHA, van Kuijk S, Ulrich DJO, van der Hulst RRWJ, Qiu SS
Affiliation: Maastricht University Medical Center; Radboud University Medical Center - The Netherlands
Journal: Nature Scientific Reports, 2024
PMID: 38278856
Key takeaways
LVA improved Lymph-ICF physical (−16.5 ± 18.5) and mental (−10.1 ± 29.5) domains at 6 months versus baseline.
No between-group difference in total Lymph-ICF score at 6 months; both groups changed minimally.
Limb volume and UEL index showed no sustained between-group differences through 6 months.
41–42% of LVA patients partially or completely stopped compression; 0% in CDT.

Background
Breast-cancer–related lymphedema (BCRL) impairs function and quality of life; complex decongestive therapy (CDT) is standard but lifelong. Supermicrosurgical LVA may improve symptoms.
Objective
Compare health-related quality of life (HrQoL) after LVA versus continued CDT in early-stage unilateral BCRL. Primary endpoint: Lymph-ICF total score.
Methods
Design/setting/LOE: Prospective multicenter RCT; Netherlands.
Participants: Adult women, unilateral BCRL, ISL stage 1–2a with viable lymphatics by ICG (Narushima II–III). Planned n = 100; interim n = 46 per arm.
Randomization: 1:1, block-stratified by site.
Interventions:
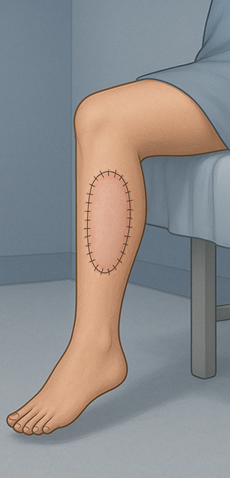
LVA: 1–5 end-to-end LVAs under microscope; patency confirmed; resume CDT maintenance after 2 weeks.
CDT: Standardized Verdonk method—skin care, MLD, exercise, compression; maintenance with elastic garment.
Primary endpoint: Lymph-ICF (lower better; ≥10-point decrease considered clinically meaningful).
Secondary endpoints: Water-displacement limb volume, UEL index, compression-garment use, adverse events/serious adverse events at 3 and 6 months.
Results
HrQoL (within-group): LVA improved physical and mental domains at 6 months (−16.46 and −10.12; p < 0.05).
HrQoL (between-group): No significant difference in total Lymph-ICF between LVA and CDT at 6 months.
Volume/circumference: No significant intergroup differences in volume or UEL index at 6 months; transient UEL improvement at 3 months in LVA not sustained.
Compression garments: At 6 months, 21.3% stopped completely and 21.7% partially in LVA (≈42% any discontinuation); 0% stopped in CDT.
Safety: Comparable adverse events; erysipelas episodes in both groups; one breast-cancer recurrence reported as SAE in LVA arm (patient remained in study).
Conclusion
At 6 months, LVA improves physical and mental aspects of HrQoL versus baseline, without measurable early limb-volume advantage over CDT; many patients reduce or stop compression after LVA. Longer follow-up is required to determine durable superiority.
Strengths & limitations
Strengths: First large multicenter RCT in BCRL assessing HrQoL after LVA; standardized CDT comparator; prespecified patient-centered outcomes.
Limitations: Interim 6-month readout; early-stage BCRL only; single LVA session; no mandated rationale for compression discontinuation; volume metrics may lag symptom change.
Clinical relevance
Offer LVA to appropriately imaged, early-stage BCRL patients primarily for symptom relief and HrQoL gains; set expectations that objective volume change may be modest by 6 months.
Discuss a trial of relaxed compression in responders, with structured monitoring for recurrence of swelling.
Critiques and questions
Endpoint alignment: The trial’s primary endpoint is total Lymph-ICF; yet benefits appeared in domain-specific scores (physical, mental).
Timing of measurement: Six months may be too early for structural changes in interstitial fibrosis to translate into measurable volume reduction; symptom relief (heaviness, tightness) often precedes volume change after LVA.
Compression policy: Compression discontinuation was frequent but not protocolized. Future analyses should correlate compression status with domain scores, infections, and rebound edema to guide tapering algorithms.
Surgical dose and imaging: One LVA session may under-treat selected patients; exploratory modeling showed no association between number of anastomoses and outcomes in this cohort, consistent with prior work. Detailing quality (ICG stage, vessel caliber) and patency over time may be more predictive than raw anastomosis count.
Generalizability: Early-stage, ICG-mappable BCRL was studied; applicability to advanced BCRL will remain uncertain until long-term data or separate trials address later stages.



Comments