Applying the modified five-item frailty index to predict complications following lower-extremity free-flap reconstruction in trauma patients
- Phil Hanwright
- Nov 14, 2025
- 2 min read
Authors: Gonzalez M, Zietowski M, Patel R, Chattha A, Cripps CN, Beederman M
Affiliation: Section of Plastic & Reconstructive Surgery, University of Chicago Medicine
Journal: Journal of Reconstructive Microsurgery, Jan 2025
PMID: 39875120
Key takeaways
The five-factor modified frailty index (mFI-5) provides a model to determine surgical risk and guide clinical decision making across specialties
The five variables include functional status, diabetes, chronic obstructive pulmonary disease, congestive heart failure and hypertension.
In 219 trauma patients, mFI-5 ≥2 was a statistically significant indicator predictive of: any complication (OR 3.83), reoperation (OR 5.39), and hematologic complications (OR 3.67).
mFI-5 = 1 was not predictive; BMI independently predicted wound infection (OR 1.09 per BMI unit).
Background
Lower-extremity trauma reconstructions have high complication rates; the role of frailty (mFI-5) as a risk stratifier in this cohort has been unclear.
Objective
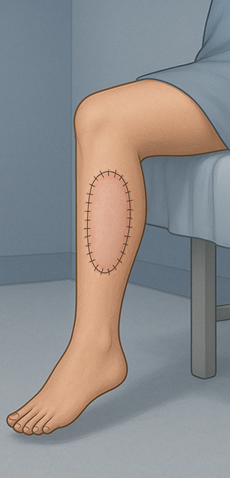
Assess whether mFI-5 predicts postoperative complications after lower-extremity free-flap reconstruction for trauma.
Methods
Design: Retrospective NSQIP analysis (2012–2020).
Cohort: n=219 trauma patients undergoing lower-extremity free flaps; grouped by mFI-5 = 0, 1, ≥2.
Outcomes (30 days): any complication, wound infection, hematologic complication (transfusion/DVT), readmission, reoperation, discharge destination, prolonged LOS.
Stats: Univariate tests + multivariable logistic regression; p<0.05.
Results
Patient profile: Mean age 47.6 ±16.2; 64.8% male. Distribution: mFI-5 0 (65.3%), 1 (25.6%), ≥2 (9.1%). Higher mFI-5 associated with older age, higher BMI, and dyspnea.
Event rates: Any complication 22.4% (49/219); readmission 6.8%; reoperation 12.3%.
mFI-5 ≥2 (vs 0):
Any complication: OR 3.829, 95% CI 1.45–10.15, p=0.007.
Reoperation: OR 5.385, 1.83–15.88, p=0.002.
Hematologic: OR 3.669, 1.27–10.64, p=0.017.
mFI-5 = 1: Not significant for any complication, wound infection, readmission, or reoperation.
Other predictors: BMI predicted wound infection (OR 1.092, p=0.014); age predicted discharge to facility (OR 1.03 per year, p=0.009).
Conclusion
In trauma patients undergoing lower-extremity free-flap reconstruction, mFI-5 ≥2 robustly identifies those at higher risk of complications, reoperation, and hematologic events. Incorporating mFI-5 into preoperative assessment can sharpen counseling and postoperative planning.
Strengths & limitations
Strengths: National dataset; focused trauma cohort; adjusted analyses demonstrating independent predictive value of mFI-5 ≥2.
Limitations: 30-day outcomes only; database constraints (e.g., flap-specific details, socioeconomic factors); modest mFI-5 ≥2 sample (n=20).
Clinical relevance
Consider frailty when completing presurgical screening for LE trauma patients: Calculate mFI-5; flag ≥2 as high risk—plan tighter hemostasis, early DVT prophylaxis, and closer monitoring.
Target modifiable risks: Address BMI-related wound risks (glucose control, nutrition, offloading) and plan resources for higher discharge support with increasing age.



Comments