Effects of Neoadjuvant Radiation and Recipient Vessel Characteristics on Microvascular Complication Rates in Reconstruction of Lower Extremity Soft Tissue Sarcoma Defects
- Phil Hanwright
- Sep 14, 2025
- 2 min read
Farmer RL, et al. Journal of Reconstructive Microsurgery, 2025. PMID: 39496317.
Key takeaways
No statistically significant increase in microvascular complications or flap loss with irradiated vessels; comparator underpowered (nonirradiated n=13; wide CI).
Perforator recipient vessels did not increase microvascular complications or flap loss as compared with named axial recipient vessels.
Postoperative venous events were most common. Plan robust outflow (two veins when feasible) and vigilant early monitoring. ≥2 venous anastomoses were performed in ~41% of cases
Background
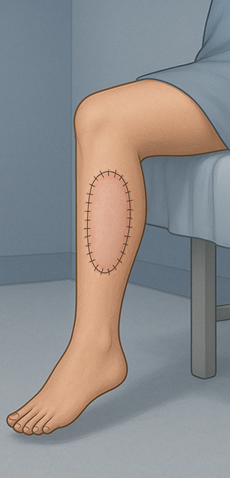
Neoadjuvant radiation with limb-sparing surgery for lower-extremity soft tissue sarcoma often creates large defects requiring free flap reconstruction. Whether irradiated or perforator recipient vessels increase microvascular risk is unclear.
Objective
Determine if recipient vessel radiation status (irradiated vs nonirradiated) and recipient vessel type (named axial vs unnamed perforator) affect microvascular complications in lower-extremity sarcoma free-flap reconstruction.
Methods
Design/LOE: Single-center retrospective cohort (Therapeutic Level III), 2009–2020.
Population: 201 patients (204 flaps) after lower-extremity soft tissue sarcoma resection; both irradiated and nonirradiated recipient vessels included.
Radiation protocol: Typically 50.4 Gy in 28 fractions; surgery performed ~9 weeks after radiation.
Cohorts: 188 (94%) reconstructions used irradiated recipient vessels; 13 (6%) used nonirradiated vessels; irradiated cohort older (mean ~59 vs ~43 years).
Interventions: All included patients underwent free-flap reconstruction (fasciocutaneous, musculocutaneous, chimeric). Standard perioperative anticoagulation (intraoperative IV heparin; postoperative SQ heparin). Staged mobilization: bedrest 48 h → sit day 3 → room ambulation day 4 → hallway walks day 6 with ACE wraps.
Endpoints: Intra-/postoperative microvascular complications needing reoperation, anastomotic revision, flap loss, or delayed healing; vessel type and radiation status recorded.
Statistics: χ² and two-sided t-tests; odds ratios with 95% CI; α = 0.05.
Results
Overall microvascular complications: 28/204 flaps (13.7%).
Timing/type: Postoperative 23/28 (82.1%); venous events 20/28 (71.4%); arterial thrombosis 4/28 (14.3%); anastomotic rupture/bleeding 4/28 (14.3%).
Irradiation status: 27/191 (14%) complications with irradiated vessels vs 1/13 (7.6%) without; OR 1.98 (0.25–15.82); P = 0.52. Flap survival 98.9% with irradiated vs 100% without.
Vessel type: No significant difference in microvascular complications between named axial and perforator recipient vessels (named 19/133 vs perforator 9/71; OR 0.87 (0.37–2.04); P = 0.75).
Anatomic distribution: Lower leg had the most events; complications distributed across groin to foot.
Practice patterns: Irradiated vessels used in ~94% of cases; perforators common in anterior/medial and posterior thigh; mean recipient vein diameter ~2.4 mm.
Conclusion
In lower-extremity sarcoma reconstruction, anastomosis to irradiated recipient vessels or to perforating branches was not associated with a statistically significant increase in microvascular complications or flap failure; interpretation should be cautious given the small sample of nonirradiated recipient vessels (n = 13).
Strengths & limitations
Large single-center series focused exclusively on lower-extremity sarcoma reconstructions.
Consistent neoadjuvant radiation regimen enhances internal consistency.
Small nonirradiated comparator (n = 13) and age imbalance may limit power and confound comparisons.
Radiation status was based on operative/clinical documentation rather than vessel histology.
Clinical relevance
For difficult lower-extremity sarcoma defects, surgeons can proceed with free flaps using irradiated vessels or perforating branches as recipients without evidence of higher flap failure. Ensure robust venous drainage and vigilant postoperative monitoring given the predominance of venous events.



Comments