Go deep or go home: Evaluating venous drainage systems in microvascular lower extremity reconstruction
- Phil Hanwright
- Nov 14, 2025
- 2 min read
Authors: Rizvi I, Kahramangil B, Wang E, Swiekatowski K, Nye JR, Trost JG, Bhadkamkar MA
Affiliation: Division of Plastic and Reconstructive Surgery, UTHealth Houston, McGovern Medical School
Journal: Journal of Reconstructive Microsurgery, Oct 2025
PMID: 41067264
Key takeaways
In 333 lower-extremity free flaps, superficial-only recipient drainage had higher venous complications than deep or combined drainage (27.8% vs 8.6% vs 4.3%).
On multivariable analysis, superficial-only increased venous-complication odds vs deep (OR 4.11, 95% CI 1.24–11.9; p=0.049); dual-vein outflow reduced odds (OR 0.34, 0.16–0.73; p=0.005).
Background
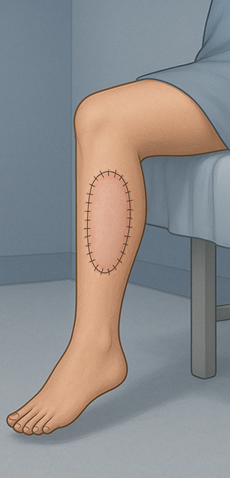
Venous congestion drives most lower-extremity flap failures. Surgeons elect to either use the deep (venae comitantes), superficial (saphenous) recipients, or both deep/superficial systems for free flap reconstruction. Comparative outcome data between the deep and superficial systems are limited.
Objective
Compare venous complications across deep vs superficial vs combined recipient drainage and by one vs two venous anastomoses.
Methods
Design/setting: retrospective review, 2016–2024, tertiary academic center.
Cohort: 333 free flaps; primary outcome = composite venous complications (congestion, hematoma, partial/total necrosis) during index hospitalization.
Groups: Deep, superficial, or combined drainage; one vs two venous anastomoses.
Analysis: Multivariable logistic regression with pre-specified covariates.
Results
Overall venous complications: 9.3% (31/333).
By drainage system: Superficial 27.8%, Deep 8.6%, Combined 4.3% (p=0.028). Superficial had more congestion and total flap necrosis than deep.
Multivariable predictors:
Superficial vs deep drainage: OR 4.11 (1.24–11.9), p=0.049.
Two veins vs one vein: OR 0.34 (0.16–0.73), p=0.005 (≈66% odds reduction).
Practice pattern: Deep 87.7% (292), Superficial 5.4% (18), Combined 6.9% (23). Two veins used in 68.2% and associated with fewer venous complications than one (p=0.004).
Clinical modifiers: Diabetes was more common in the complication group (29.0% vs 10.6%; p=0.007). Flap type also mattered: higher odds with larger flaps such as the latissimus dorsi (OR 5.29) and ALT (OR 3.73) vs radial forearm.
Conclusion
For lower-extremity reconstruction, prioritize deep venous recipients; avoid superficial-only drainage when possible. Consider dual-vein outflow to reduce venous complications, especially in high-risk settings.
Strengths & limitations
Strengths: Contemporary, sizable cohort; clear drainage definitions; adjusted analysis identifying drainage system and number of veins as independent predictors.
Limitations: Retrospective, single-center; small superficial-only sample; limited detail on vein size/zone-of-injury—selection bias possible; surgeons preferentially used deep system when available.
Clinical relevance
Choose deep first. Use venae comitantes as primary recipients; if superficial system is needed, prefer combined over superficial-only.
Favor two veins when feasible (trauma, bulky flaps, diabetes) to lower venous risk.



Comments