Intraoperative Peripheral Frozen Margin Assessment in Soft Tissue Sarcoma
- Phil Hanwright
- Jul 1, 2025
- 1 min read
Updated: Jul 1, 2025
Key Takeaways
Intraoperative frozen margins only changed management in
Paper Info
Journal of Surgical Oncology, Vol 131, 2025, pp 694-698; accepted 10 Sep 2024.
Background
Intra-operative frozen-section assessment of peripheral margins is traditional in musculoskeletal oncology, yet evidence in soft-tissue sarcoma (STS) is sparse.

Objective
Quantify practice patterns, clinical impact, and cost-utility of peripheral-margin sampling (Frozen and Permanent) during STS resection.
Methods
Retrospective review (2005-2019), multi-institutional
Inclusion:
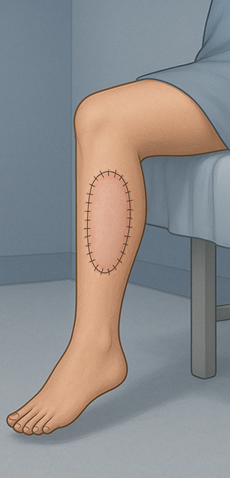
Extremity or truncal soft tissue sarcoma
Primary tumor
≥ 2 years follow up
Exclusion:
Osseous disease
Re-excisions
Pathology charges were evaluated to determine cost of margin assessment
Results
A total of 179 patients were included
119 (66%) had peripheral margins sent (frozen or permanent)
Frozen margin n = 27 (23%)
Permanent margin n = 92 (77%)

Only 1 case in which frozen margins were sent returned positive, resulting in a wider resection at the time of initial surgery
On average, sending margins added approximately $5,000, not including OR time
Conclusion
Routine peripheral-margin sampling provides limited actionable information, modest diagnostic agreement, and substantial cost. A selective, indication-based approach is recommended.
Strengths & Limitations
Strengths: Multi-institution, includes diverse STS subtypes.
Limitations: Retrospective, under-powered for outcome correlations.



Comments